
Additional inclusion criteria included history of seizures and EEG and MRI studies performed at our institution. Patients without confirmatory testing or where there was diagnostic ambiguity were excluded. Patients with a definite, genetically confirmed diagnosis of mitochondrial disorder were included. Patients were classified based on previously published diagnostic criteria as having a definite, probable, or possible mitochondrial disorder ( 20– 23). Records were reviewed for diagnosis, history of epilepsy, laboratory investigations, and available raw EEG and MRI studies. This retrospective study was performed using the Mayo Clinic Mitochondrial Disease Database from January 2011 to December 2019. A secondary objective was to study nutraceutical therapy use in relationship to disease progression. The main objective of this study was to evaluate the EEG, clinical, and radiologic progression of disease in patients with epilepsy due to mitochondrial cytopathies in order to identify features, which may help the clinician more readily diagnose these disorders. These nutraceutical therapies, sometimes referred to as the “mitochondrial cocktail,” are unproven at present with limited evidence-based support of their use. Treatment of these disorders is limited and mainly comprised of utilization of nutritional therapies aimed to increase the metabolic substrates used in mitochondrial processes ( 19). The time to diagnosis can be variable and in some cases may take years when presentations are atypical or when symptoms and diagnostic studies are non-specific. Within the central nervous system, mitochondrial dysfunction frequently results in structural injury, which can manifest as characteristic neuroimaging abnormalities ( 17, 18).

While seizures are not unique to a mitochondrial etiology ( 11– 13), it has been previously noted that EEG abnormalities in these disorders tend to have a posterior cerebral predilection ( 14– 16). Published information on specific seizure semiology and electroencephalogram (EEG) findings in mitochondrial disorders is limited compared to what is known about other genetic and metabolic epilepsies, likely owing to the significant variability between and within specific mitochondrial disorders ( 10).

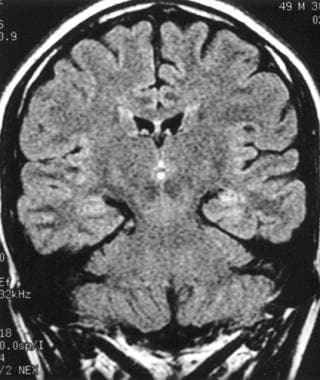
Seizures are particularly common in mitochondrial disorders such as polymerase gamma (POLG) mutations, mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS), and myoclonic epilepsy with ragged-red fibers (MERRF) ( 6– 9). The central nervous system is particularly susceptible to mitochondrial defects and neurologic manifestations are frequently seen in mitochondrial disorders ( 4, 5). Additional study is needed on nutraceutical supplementation in mitochondrial disorders.ĭisorders of mitochondrial function and metabolism result in energy failure producing varying severity of symptoms ( 1– 3). Focal seizures and focal status epilepticus with visual symptoms were common. Over time, electroencephalogram (EEG) and imaging abnormalities increasingly occurred over the posterior cerebral regions.
#Seizures with normal eeg and mri series#
At last follow-up, eight patients were deceased and the remainder had moderate-to-severe disability.ĭiscussion: In this series of patients with epilepsy and mitochondrial disorders, we found increased propensity for seizures arising from the posterior cerebral regions. All the patients were on nutraceutical supplementation with no significant change in disease progression seen. Abnormalities over the posterior cerebral regions were seen in 66% of ictal recordings and 44% of imaging studies. Status epilepticus occurred in 15 patients, with focal status epilepticus in 13 patients, including 9 patients with visual features. Results: A total of 20 patients (14 females, 6 males) aged 0.5–61 years with epilepsy and genetically confirmed mitochondrial disorders were identified.

A total of 164 patients were reviewed with 20 patients fulfilling inclusion criteria. Methods: This is a retrospective case series from January 2011 to December 2019 at a tertiary referral center of patients with epilepsy and a genetically confirmed diagnosis of a mitochondrial disorder. In this study, we evaluated clinical, electrophysiologic, and imaging features in patients with epilepsy and mitochondrial disorders to identify common features, which could aid in earlier identification of a mitochondrial etiology. Epilepsy can be a presenting symptom with several mitochondrial disorders. 3Department of Clinical Genomics, Mayo Clinic, Rochester, MN, United Statesīackground: Identification of an underlying mitochondrial disorder can be challenging due to the significant phenotypic variability between and within specific disorders.2Department of Radiology, Mayo Clinic, Rochester, MN, United States.1Department of Neurology, Mayo Clinic, Rochester, MN, United States.


 0 kommentar(er)
0 kommentar(er)
